Carcinoma basocelular
Carcinoma basocelular
Almost all BCCs occur on parts of the body excessively exposed to the sun — especially the face, ears, neck, scalp, shoulders, and back. On rare occasions, however, tumors develop on unexposed areas. In a few cases, contact with arsenic, exposure to radiation, open sores that resist healing, chronic inflammatory skin conditions, and complications of burns, scars, infections, vaccinations, or even tattoos are contributing factors. It is not possible to pinpoint a precise, single cause for a specific tumor, especially one found on a sun-protected area of the body or in an extremely young individual.
Anyone with a history of sun exposure can develop BCC. However, people who are at highest risk have fair skin, blond or red hair, and blue, green, or grey eyes. The tendency to develop BCC may also be inherited. Those most often affected are older people, but as the number of new cases has increased sharply each year in the last few decades, the average age of patients at onset has steadily decreased. The disease is rarely seen in children, but occasionally a teenager is affected. Dermatologists report that more and more people in their twenties and thirties are being treated for this skin cancer.
Anyone with a history of sun exposure can develop BCC. However, people who are at highest risk have fair skin, blond or red hair, and blue, green, or grey eyes. The tendency to develop BCC may also be inherited. Those most often affected are older people, but as the number of new cases has increased sharply each year in the last few decades, the average age of patients at onset has steadily decreased. The disease is rarely seen in children, but occasionally a teenager is affected. Dermatologists report that more and more people in their twenties and thirties are being treated for this skin cancer.
Men with BCC have outnumbered women with the disease, but more women are getting BCCs than in the past. Workers in occupations that require long hours outdoors and people who spend their leisure time in the sun are particularly susceptible.
People who have had one BCC are at risk for developing others over the years, either in the same area or elsewhere on the body. Therefore, regular visits to a dermatologist should be routine so that not only the site(s) previously treated, but the entire skin surface can be examined.
Should a cancer recur, the physician might recommend a different type of treatment. Some methods, such as Mohs micrographic surgery, may be highly effective for recurrences.
WARNING SIGNS
Frequently, two or more of these features are present in one tumor. In addition, BCC sometimes resembles noncancerous skin conditions such as psoriasis or eczema. Only a trained physician, such as a specialist in diseases of the skin, can decide for sure. If you observe any of the warning signs or some other worrisome change in your skin, consult your physician immediately.
A Scar-like Area
A scar-like area that is white, yellow or waxy, and often has poorly defined borders; the skin itself appears shiny and taut. This warning sign may indicate the presence of an invasive BCC that is larger than it appears to be on the surface.
An Open Sore
An open sore that bleeds, oozes, or crusts and remains open for a few weeks, only to heal up and then bleed again. A persistent, non–healing sore is a very common sign of an early BCC.
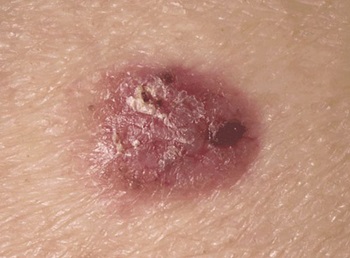
A Reddish Patch or Irritated Area
A reddish patch or irritated area, frequently occurring on the face, chest, shoulders, arms, or legs. Sometimes the patch crusts, and it may also itch. At other times, it persists with no noticeable discomfort.
A Shiny Bump or Nodule
A shiny bump or nodule that is pearly or translucent and is often pink, red, or white. The bump can also be tan, black, or brown, especially in dark-haired people, and can be confused with a mole.
A Pink Growth
A pink growth with a slightly elevated rolled border and a crusted indentation in the center. As the growth slowly enlarges, tiny blood vessels may develop on the surface.
A Scar-like Area
A scar-like area that is white, yellow or waxy, and often has poorly defined borders; the skin itself appears shiny and taut. This warning sign may indicate the presence of an invasive BCC that is larger than it appears to be on the surface.
An Open Sore
An open sore that bleeds, oozes, or crusts and remains open for a few weeks, only to heal up and then bleed again. A persistent, non–healing sore is a very common sign of an early BCC.
TREATMENT OPTIONS
After the physician’s examination, the diagnosis of BCC is confirmed with a biopsy. In this procedure, the skin is first numbed with local anesthesia. A sample of the tissue is then removed and sent to be examined under a microscope in the laboratory to seek a definitive diagnosis. If tumor cells are present, treatment is required. Fortunately, there are several effective methods for eliminating BCC. Choice of treatment is based on the type, size, location, and depth of penetration of the tumor, the patient’s age and general health, and the likely outcome to his or her appearance.
Treatment can almost always be performed on an outpatient basis in the physician’s office or at a clinic. With the various surgical techniques, a local anesthetic is commonly used. Pain or discomfort during the procedure is minimal, and pain afterwards is rare.
ED&C ELECTRODISECATION AND CURETTAGE
This technique is usually reserved for small lesions. The growth is scraped off with a curette, an instrument with a sharp, ring-shaped tip), then the tumor site is desiccated (burned) with an electrocautery needle. The procedure has cure rates generally above 95 percent. In some areas of the body, it is repeated a few times to help assure that all cancer cells are eliminated. Local anesthesia is required. The technique may not be as useful for aggressive BCCs, those in high-risk sites, or sites that would be left with cosmetically undesirable results. Typically, a round, whitish scar is left at the surgery site.
MOHS SURGERY
A physician trained in Mohs micrographic surgery removes a thin layer of tissue containing the tumor. While the patient waits, frozen sections of this excised layer are mapped in detail and examined under a microscope, generally in an on-site laboratory. If cancer is present in any area of the excised tissue, the procedure is repeated only on the body area where those cancer cells were identified (the tissue mapping allows the Mohs surgeon to pinpoint this area of the body), until the last excised layer viewed microscopically is cancer-free. This technique can save the greatest amount of healthy tissue and has the highest cure rate, 99 percent or better. It is often used for large tumors in cosmetically important areas, and those that have recurred, are poorly demarcated (hard to pinpoint), or are in critical areas around the eyes, nose, lips, and ears, temple, scalp, or fingers.
This kind of Surgery is not available in Puerto Vallarta, but we can refer you to other cities in Mexico where they do Mohs Surgery
EXCISIONAL SURGERY
Using a scalpel, the physician removes the entire growth along with a surrounding border of apparently normal skin as a safety margin. The skin around the surgical site is closed with stitches, and the tissue specimen is sent to the laboratory to verify that all cancerous cells have been removed. Cure rates are generally above 95 percent in most body areas, similar to those of curettage and electrodessication. A repeat excision may be necessary on a subsequent occasion if evidence of skin cancer is found in the specimen.
CRYOTHERAPY
Tumor tissue is destroyed by freezing. Liquid nitrogen is applied to the growth with a cotton-tipped applicator or spray device, freezing it without requiring any cutting or anesthesia (though a local anesthetic can be used, since the technique often involves a modest amount of pain). The procedure may be repeated at the same session to ensure total destruction of malignant cells. The growth subsequently blisters or becomes crusted and falls off, usually within weeks. Temporary redness and swelling can occur, and in most cases, pigment may be lost at the site. Cryosurgery is effective for the most common tumors, especially superficial BCC, and is useful for patients with bleeding disorders or intolerance to anesthesia. This method is used less commonly today, and has a lower cure rate than the surgical techniques–approximately 85-90 percent, depending on the physician’s expertise.
LASER
Some lasers vaporize (ablate) the skin’s top layer to destroy lesions. Others (non-ablative lasers) penetrate the skin without removing the top layer; one such laser has been shown in some cases to treat small, superficial BCCs successfully. Laser therapy is not yet FDA-approved for BCC, but is sometimes used as a secondary therapy when other techniques are unsuccessful.
TOPICAL MEDICATIONS
These creams, gels, or solutions are used to treat limited, specific BCCs.
Imiquimod is FDA-approved only for superficial BCCs, with cure rates generally between 80 and 90 percent. The cream is rubbed gently into the tumor five times a week for up to six weeks or longer. The first in a new class of drugs that work by stimulating the immune system, it causes the body to produce interferon, a chemical that attacks cancer.
5-Fluorouracil (5-FU), a chemotherapy drug approved to treat internal cancers, also has been FDA-approved for superficial BCCs, with similar cure rates to imiquimod. The liquid or cream is gently rubbed into the tumor twice a day for three to six weeks. Side effects are variable, and some patients do not experience any discomfort, but redness, irritation, and inflammation usually occur.
It is important to note that (unlike Mohs surgery and excisional surgery), curettage and electrodessication, radiation, cryosurgery, and topical medications all have one significant drawback in common – since no tissue is examined under the microscope, there is no way to determine how completely the tumor was removed.
NEW ORAL TREATMENT FOR ADVANCED BASAL CELL CARCINOMA
ErivedgeTM (vismodegib) was approved by the FDA in 2012 for extraordinarily rare cases of metastatic BCC or locally advanced BCC that become dangerous and even life-threatening. The first medicine ever for advanced BCC, it works by blocking the “Hedgehog” signaling pathway, which is a key step in the development of BCC. It is approved only for very limited circumstances where the nature of the cancer precludes other treatment options (such as surgery or radiation). Several other targeted Hedgehog inhibitors are also being investigated as potential treatments for locally advanced and metastatic BCC. Due to a risk of birth defects, vismodegib should not be used by women who are pregnant or may become pregnant. Birth control must be used by couples if the woman is capable of becoming pregnant.
While BCCs and other skin cancers are almost always curable when detected and treated early, it is best to prevent them in the first place. Make these sun safety habits part of your daily health care routine:
- Seek the shade, especially between 10 AM and 4 PM.
- Do not burn.
- Avoid tanning and never use UV tanning beds.
- Cover up with clothing, including a broad-brimmed hat and UV-blocking sunglasses.
- Use a broad spectrum (UVA/UVB) sunscreen with an SPF of 15 or higher every day. For extended outdoor activity, use a water-resistant, broad spectrum (UVA/UVB) sunscreen with an SPF of 30 or higher.
- Apply 1 ounce (2 tablespoons) of sunscreen to your entire body 30 minutes before going outside. Reapply every two hours or after swimming or excessive sweating.
- Keep newborns out of the sun. Sunscreens should be used on babies over the age of six months.
- Examine your skin head-to-toe every month.
- See your doctor every year for a professional skin exam.


STAFF
NURSE GRADUATED FROM CUC
CERTIFICATE PROGRAM IN WOUND HEALING
Monica
Padilla

STAFF
RECEPTION AND SALES
Betsy
Aguirre

Marisol
Pelayo

STAFF
CERTIFIED COSMETOLOGIST



STAFF
CERTIFIED COSMETOLOGIST
Esmeralda
Alcaraz
ADDRESS
Derma Health Av. Los Tules 158, Col. Díaz Ordaz Puerto Vallarta
SCHEDULE
- Mon-Fri 9:00 am a 5:00 pm
- Saturday 9:00 am a 14:00 pm
- Sunday closed
- Copyright 2025. All rights reserved.